Contents
- 1 Medical disclaimer
- 2 Why home monitoring matters (in plain English)
- 3 The goal: fewer ‘random’ numbers and more useful averages
- 4 Step 1: Choose the right monitor (this matters more than people think)
- 5 Step 2: Learn the ‘golden rules’ of accurate readings
- 6 Step 3: Use a simple schedule (so you don’t overthink it)
- 7 Morning vs night: does it matter?
- 8 How to average your readings
- 9 Common mistakes and the quick fix
- 10 When to contact a clinician
- 11 How this connects to your Nitric Oxide (NO) strategy
- 12 References
Medical disclaimer
This article about home blood pressure monitoring is for educational purposes only and is not medical advice. If you have high blood pressure, heart disease, kidney disease, are pregnant, or take prescription medications, talk with a qualified clinician before changing treatment. Do not stop or adjust blood pressure medication without your prescriber.
Why home monitoring matters (in plain English)
A clinic blood pressure reading is a snapshot. Home blood pressure monitoring gives you a trend — and trends are what help you and your clinician make good decisions. The American Heart Association recommends home monitoring for many people with hypertension and emphasizes using an automatic, upper‑arm cuff.[1]
The goal: fewer ‘random’ numbers and more useful averages
Most beginners get confused because blood pressure naturally moves up and down. The fix is simple: use a consistent technique and compare weekly averages, not single readings.[2][6]
Step 1: Choose the right monitor (this matters more than people think)
AHA’s general advice: choose an automatic, upper‑arm cuff device.[1]
Smart Connectivity: Keep track of your blood pressure readings with ease using the RENPHO wireless blood pressure monitor. Simply connect it to the Renpho Health app on your iOS or Android device, and you'll be able to store and view your historical measurement data and track your progress on a daily, weekly, monthly, or yearly basis.
| What to look for | Why it matters | Beginner tip |
| Upper‑arm cuff | Wrist devices are more sensitive to positioning and can be less reliable for many users. | Start with upper‑arm unless your clinician says otherwise. |
| Correct cuff size | A cuff that’s too small or too large can distort readings. | Measure mid‑upper arm circumference and match the cuff size on the box. |
| Validated device | Validation means it has been tested for accuracy. | If unsure, ask your pharmacist/clinician for a validated model. |
| Memory/app (optional) | Helps reduce logging errors and “missing” readings. | Nice-to-have, not required. |
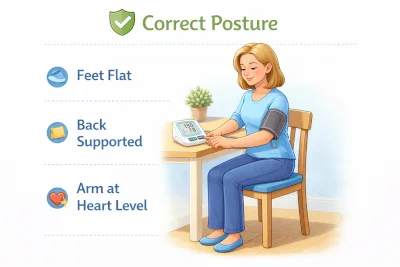
Step 2: Learn the ‘golden rules’ of accurate readings
These steps are repeated across AHA instructions and measurement guides.[2][3][4]
- Rest quietly for 5 minutes before measuring.
- Sit upright with back supported, feet flat, legs uncrossed.
- Arm supported at heart level (on a table).
- Cuff on bare upper arm (not over clothing).
- Do not talk during the measurement.
- Take at least 2 readings, 1 minute apart, and record both (or the average).[2]
Table: Quick setup checklist (print this mentally)
| Before | During | After |
| No caffeine/exercise/smoking right before if possible | Stay still and quiet | Record both readings |
| Bladder empty if you can | Do not talk | Note time + meds + symptoms |
| Rest 5 minutes seated | Arm supported at heart level | Use weekly averages |
Step 3: Use a simple schedule (so you don’t overthink it)
A common research and guideline-friendly pattern is the “7‑day” style schedule: two readings in the morning and two in the evening (often called a 7‑day home BP schedule).[5][6]
| Schedule option | Who it’s for | What to do |
| Beginner (3 days) | You want a quick baseline | Morning + evening, 2 readings each time. Average the last 2–3 days. |
| Standard (7 days) | Best mix of accuracy + practicality | Morning + evening, 2 readings each time. Average all days (many protocols exclude day 1). |
| Maintenance | You’re stable and tracking | A few days per month, or as clinician recommends. |
Morning vs night: does it matter?
For most people, what matters most is consistency. Many protocols use morning and evening to capture how BP behaves across the day.[5][6] You’ll learn more from stable habits than from chasing the “perfect” time.
How to average your readings
Use this simple rule: ignore single spikes and look at the average.
Beginner method:
1) Take 2 readings, 1 minute apart (AM and PM)
2) Write down both
3) At the end of the week, average all readings (or average the daily AM/PM averages).[2][6]
Example BP log (copy into Notes app)
| Date | AM reading 1 | AM reading 2 | PM reading 1 | PM reading 2 | Notes (meds/symptoms) |
| Mon | — | — | — | — | — |
| Tue | — | — | — | — | — |
| Wed | — | — | — | — | — |
| Thu | — | — | — | — | — |
| Fri | — | — | — | — | — |
| Sat | — | — | — | — | — |
| Sun | — | — | — | — | — |
Common mistakes and the quick fix
When to contact a clinician
If you have symptoms like chest pain, severe shortness of breath, fainting, or neurologic symptoms, seek urgent care. For concerning but non-emergency trends, share your home averages and your log with your clinician. AHA emphasizes sharing recorded results with your care team.[2]
How this connects to your Nitric Oxide (NO) strategy
Home monitoring is how you know whether your nitric oxide plan (greens, walking, mouthwash habits, supplements) is actually helping. Use a 2‑week “one change at a time” approach so you can tell what moved the needle.
Recommended Reading
- Nitric Oxide for Blood Pressure
- Nitric Oxide and Blood Pressure: What It Does and What to Track
- 12 Natural Ways to Support Nitric Oxide for Healthier Blood Pressure
References
- [1] American Heart Association. Home Blood Pressure Monitoring. (Updated Aug 14, 2025). https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings/monitoring-your-blood-pressure-at-home
- [2] American Heart Association. Home Blood Pressure Measurement Instructions (PDF). (Copyright 2025). https://www.heart.org/-/media/files/health-topics/high-blood-pressure/how_to_measure_your_blood_pressure_letter_size.pdf
- [3] American Heart Association News. Monitoring blood pressure at home can be tricky. Here’s how to do it right. (May 23, 2022). https://www.heart.org/en/news/2022/05/23/monitoring-blood-pressure-at-home-can-be-tricky-heres-how-to-do-it-right
- [4] Mayo Clinic. How to measure blood pressure using an automatic monitor (video/guide). https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/multimedia/how-to-measure-blood-pressure/vid-20084749
- [5] Niiranen TJ, et al. Optimal Schedule for Home Blood Pressure Measurement. Hypertension. 2011. https://www.ahajournals.org/doi/10.1161/hypertensionaha.110.162123
- [6] Lin HJ, et al. Standardized home blood pressure monitoring (“722” protocol). Front Cardiovasc Med. 2022. https://pmc.ncbi.nlm.nih.gov/articles/PMC9532917/
Last updated: 2026-01-03

