Contents
Fungal infections of the skin have a tendency to be persistent but seldom form true pus or cause fever. Fungi are more complex than bacteria and multiply through spores. In general, these infections do not respond to antibiotics. Some are extremely common, and most have at least one fungal infection.
The most common fungal infections of the skin are ringworms (dermatophytosis), yeast infections (candidiasis), and tinea versicolor (changing color).
Ringworm Infections: One of the Most Common Fungal Infections of the Skin

Ringworm infections (tinea) are not caused by a worm, as the name suggests, but by fungi. The term ringworm stems from the observation that the lesions tend to heal at their centers and continue to spread in a widening, ringlike fashion.
Although these infections spread by contact with infected objects used by others (towels, combs, etc.), the affected person probably has an inherited inability to combat a particular fungus. This is why only certain people develop the disease in a camp or family.
Fungal Infections of the Skin: Athletes Foot (tinea pedis)
This infection is a ringworm occurring between the toes in which the skin softens, turns white, and tends to peel and flake. Blisters and cracks appear. Secondary infection is common, resulting in the formation of ulcers and pus with itching and burning.

Athlete’s foot is probably the most common infection of the skin. It is contagious and spreads from dirty shoes, showers (primarily public), and areas surrounding swimming pools. The hands may be affected in two ways:
- Painless “blisters” develop on both hands as an allergic response to toxins produced by the infection in the feet (carried in the blood to the hands—dermatophytid reaction).
- The fungus also affects the scaling of one hand (2 feet, I hand disease).
The best thing to do is wash your feet daily (or more often), dry thoroughly between the toes, use an antifungal powder (antifungal creams tend to keep the skin moist), use absorbent socks, and, whenever possible, wear sandals and air your feet. Should the problem continue, see your physician for systemic medicine.
Ringworm of the Scalp, Body, and Groin (Tinea Capitis, Corporis, T. Cruris)
Ringworm of the scalp—most common in children—presents small, round, reddish, scaly spots with blisters. The area enlarges rapidly, becomes grayish, and shows definite boundaries. The affected hair shafts break off, and patchy hair loss results.

Ringworms of the body may affect all areas of the skin except the scalp and groin. It first appears as pea-sized reddened patches, which, while increasing, heal in the center, forming rings. The outer edges show tiny bumps and small blisters. There is mild itching.
Ringworm of the groin (jock itch or crotch itch) presents brownish-red scaly patches with tiny blisters at the spreading edges. There are mild itching and smarting. It affects the inner surfaces of the upper thighs and the genital and anal areas. Heat, moisture, profuse sweating, and chafing by clothing aggravate the infection. This disorder is seen more frequently in men.
Ringworm of the beard (barber’s itch) is an inflammation in and around the hair follicles. Superficial nodules appear in groups, become deep-seated, have thin discharge pus and irritation, and are mildly painful.
Ringworm of the nails affects either fingernails or toenails, which become thickened, brittle, broken, white, and often ridged. Frequently, only one nail is affected.
After an appropriate diagnosis, your physician can prescribe an ointment containing fungicide or an oral antibiotic (griseofulvin is commonly used, as it is secreted through the skin). Some fungal infections (of the beard and nails) tend to be persistent; hence, their treatment will be prolonged. In the ringworm of the beard, hairs should be clipped, not shaved.
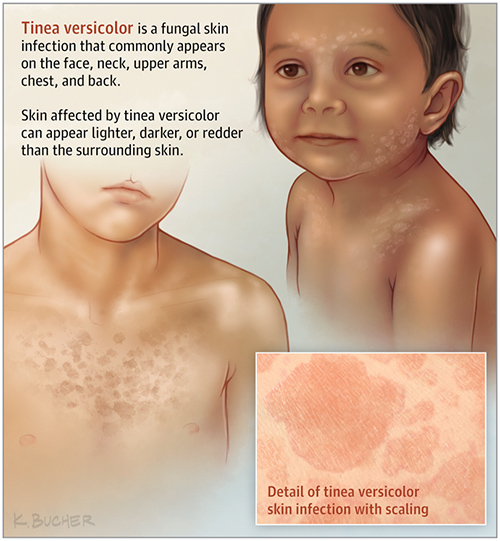
Tinea Versicolor (Sun Fungus)
This fungus is a curious but harmless skin infection that affects some young adults. The lesions are small, rounded, velvety, flat spots that scale and itch slightly. The yeast organism attacks the skin’s pigment-producing cells on the chest, shoulders, armpits, and abdomen.
The spots may lose their pigment and not tan or become pigmented (hence the name “tinea versicolor”). Treatment consists of an antifungal medication by mouth, antifungal creams, sulfur/salicylic soap, or shampoo.
Yeast Infections
Yeast organisms (species of candida) cause infections (candidiasis) in the mouth (thrush), fingernail folds, body folds, and areas around the vagina and anus. Whitish curd-like deposits develop or red, raw lesions. These may be mild burning and itching. Warmth and moisture aggravate the condition.
This benign organism—found in the mouth, vagina, and intestine—does not normally inhabit the skin. For reasons unknown, the organism may cause severe infections in debilitated people, in those taking antibiotics by mouth for an extended period, in women taking birth control pills, in those obese, in diabetics, and in those who sweat profusely. Skin folds should be kept dry. Ask your physician for advice as to the best cream for fungal infections.
DISCLAIMER: All content on this website is presented solely for educational and informational objectives. You should not rely on the information provided as a replacement for advice, diagnosis, or treatment from a qualified medical expert. If you are pregnant, nursing, or have any preexisting medical concerns, you should talk to your doctor before using any herbal or natural medicines.
REFERENCES
- Hardinge, Mervyn G and Harold Shryock. “Family Medical Guide.” Hardinge, Mervyn G and Harold Shryock. Family Medical Guide. Ed. Marvin Moore and Bonnie Tyson-Flynn. Vol. Three. Oshawa; Washington, D.C.; Hagerstown: Pacific Press Publishing Association; Review and Herald Publishing Association, 1999. Three vols. 251, 252, 253. Print. [fungal infections of the skin]
- National Institutes of Health (NIH): https://www.niaid.nih.gov/diseases-conditions/fungal-diseases
- Centers for Disease Control and Prevention (CDC): https://www.cdc.gov/fungal/index.html
